TMJ
Home | Our Procedures | TMJ
What is TMJ?
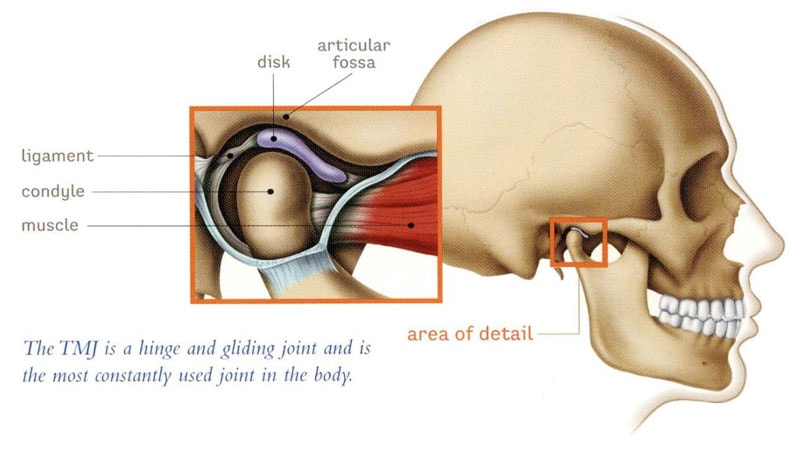
The temporomandibular joint (TMJ) is located in front of the ear and is formed by the portion of lower jaw bone that is the moving the part of the joint as you open and close your mouth (condyle of the mandible) and the base of the skull (glenoid fossa). In between the lower jaw and the base of the skull should be a disc that acts a cushion and allows for smooth, pain free movement of the joint. Problems with the TMJ often arise if this disc is in the wrong place (dislocated), and can result in arthritis (inflammation of the joint) in some cases. Other conditions affecting the TMJ may include: tumors, systemic conditions (rheumatoid arthritis), dislocations of the joint, fusion of the joint to the base of the skull (ankylosis), growth disturbances of the condyle (condylar hyperplasia or resorption), or trauma (fractures of the lower jaw bone in or near the joint). The most common cause of pain in the TMJ is disc disorders and arthritis.

Common TMJ Disorders
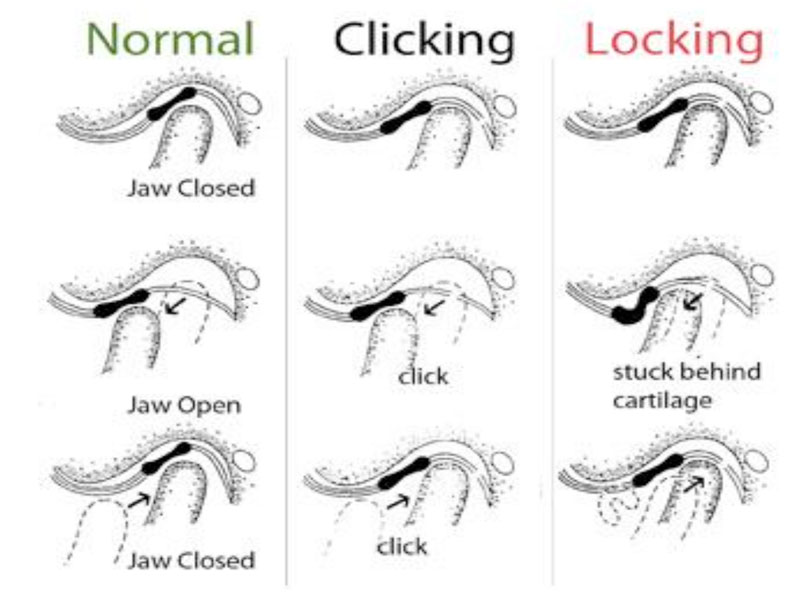
- Anterior disc dislocation with reduction- disc sits out front when closed, but pops/clicks into place on opening. May cause joint noises or open lock (jaw gets stuck open)
- Anterior disc dislocation without reduction- disc sits out front when closed and stays out front as you open. May cause closed lock (inability to fully open mouth)
- Perforations of the disc- grating/crunching/grinding sounds in joint
- Arthritis- inflammation of the joint that results in changes in the disc and bones of the joints
- Chronic dislocation of the joint
Pain can result from the above listed issues within the joint, but can also be due to other conditions such as night time clenching (bruxism), muscle pain/spasms (myofascial pain), or chronic pain conditions affecting the muscles of the face and neck (such as fibromyalgia). These conditions can cause or exacerbate joint issues, and must be appropriately treated in conjunction with the TMJ issue. However, bruxism, myofascial pain, and chronic pain issues are nonsurgical issues, and are typically managed with medications, mouth splints, and physical therapy.
Treatment of TMJ
The treatment of TMJ problems may include first trying conservative therapy such as soft/no chew diet, warm compresses over the joints, anti-inflammatory medications (Ibuprofen, Aleve, etc.), muscle relaxants, and reducing bruxism (medications, splints, bite adjustments by dentist, etc.). If no improvement occurs in 6-8 weeks, advanced imaging such as CT scan or MRI may be ordered to fully evaluate the joint. Based on the imaging, surgical procedures may be recommended including:
- Arthrocentesis- flushing out the joint under sedation performed in the office.
- Arthroscopy- putting a small camera in the joint to look at the condition of the joint/disc
- Arthroplasty- incision in front of the ear to access the joint to allow for repositioning of thedisc or reshaping the bones.
- Modified condylotomy- making a small cut in the lower jaw bone to allow for more space forthe disc to reposition naturally. This involves having the jaw wired together for a brief period of time to allow the bone cut to heal without changing how the teeth fit.
- Orthognathic surgery- making small cuts in the lower (and sometimes upper) jaw bone to reposition the jaws into a better relationship. This involves orthodontic treatment (braces or sometimes invisalign) before and after surgery.
- Total joint replacement- replacement of the condyle and fossa with prosthetic components (similar to a knee or hip replacement).
The goal of any TMJ surgery is to improve function and reduce pain. It is often not possible to completely eliminate pain in the TMJ; however, with thorough discussion and individualized treatment planning, many patients can achieve improvement in function and reduction in pain that significantly improves the overall quality of life.
