Blog
What is PRF? How Does it Help with Oral Surgery?
There are many small steps that surgeons take to ensure surgery goes [...]
What are Dental Bone Graphs?
A dental bone graft is a surgical procedure to repair or rebuild [...]
Home Care Tips After Tooth Extractions
If you’re planning to get teeth extracted, it’s important to take the [...]
What is Anesthesia?
Anesthesia Services A lot of people get nervous to visit the dentist [...]
What is Mandibular Tori?
Torus Mandibularis (mandibular or dental tori) are bone growths that develop on [...]
Oral Pathology Vs. Oral Cancer
When visiting a dentist or doing an oral examination, the discovery of [...]
Oral Cancer Risk Factors
Understanding your risk for oral cancer allows for early detection and prompt [...]
Danger and Symptoms of Oral Cancer
132 new people in the US are diagnosed with oral cancer every [...]
How Long Does it Take to Get an Implant?
Implant Timeline A Dental Implant is a surgical component that fuses with [...]
What is a Dental Implant?
To put it simply, a dental implant is an artificially placed root [...]
Why Do You See an Oral Surgeon for Facial Trauma?
Facial trauma can be simply described as any injury or damage to [...]
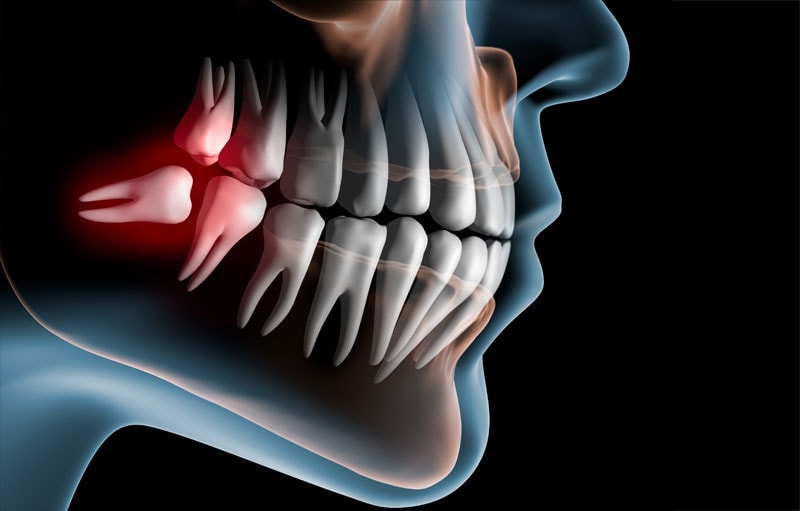
What Are Impacted Wisdom Teeth?
9/10 people have at least one impacted wisdom tooth! This is the [...]
Do My Wisdom Teeth Need to be Removed?
Wisdom teeth are your third molars set in the back of your [...]
What is an Oral Surgeon?
Knowing when to visit a dentist is easy, but Oral Surgeons have [...]